'The
entire medical profession is too terrified to denounce this rubbish'
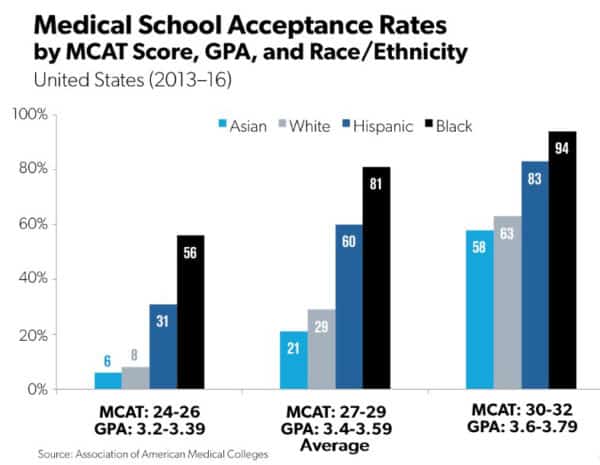
But let’s start with qualifications. Here are data for doctors who are just starting to practice now.
The figures are in three groups according to qualifications. The bars on the left were the chances of getting into medical school with a low MCAT score – that’s the Medical College Acceptance Text – of 24 to 26 and a GPA of only 3.2 to 3.39. Asians – the light blue bar – had only a 6 percent chance of being admitted, and whites, in gray, had an 8 percent chance. But Hispanics with low scores and grades – the dark blue bar – had a 31 percent chance and blacks had a 56 percent chance of getting in. Look at the results for the better qualified applicants. Being black or Hispanic is a huge advantage.
This has been the case for decades, but a thick new form of madness has spread over medicine: an anti-racism rampage that has several goals. Turn more blacks and Hispanics into doctors, no matter what. Make sure everyone in medicine is battling “structural racism” and “white supremacy” every moment of the day. Blame society – and especially white doctors – for the bad health of “people of color.” “Center” treatment of non-whites, which means treat them better. And, of course, persecute anyone who opposes this craziness.
It’s a matter of blind faith that “underrepresented minorities” – that’s blacks and Hispanics and sometimes American Indians – are just as smart and hard-working as whites and Asians – Asians are the over-represented minority. And that’s why people write articles like this with a straight face: “The Consequences of Structural Racism on MCAT Scores and Medical School Admissions.”
The article sorrows over low black and Hispanic scores, and even admits the test isn’t biased. It then asserts, as if by divine revelation, that the problem is “structural racism.” Ability has nothing to do with it. Medical schools should junk the MCAT or at least realize that low-scoring blacks and Hispanics will make wonderful doctors who will lead the fight against structural racism.
That’s why “Penn Medical School Expands Minority-Candidate Program That Does Not Require MCAT.”
Preferred minorities can skip the test and be admitted with a GPA of 3.2 instead of the usual 3.89.
Here’s another crazy article: “Association Between Resident Race and Ethnicity and Clinical Performance Assessment Scores.”
It bravely reports that Black and Hispanic doctors in residency training score worse than whites on every standard of evaluation. There’s not a single area in which they are even as good. The authors can think of only three possible reasons: “bias in faculty assessment, effects of a noninclusive learning environment, or structural inequities in assessment.”
Forget about how much standards were lowered just to get them into med school. Don’t even imagine there could be such a thing as race differences in average IQ. Their bad evaluations cannot be their fault.
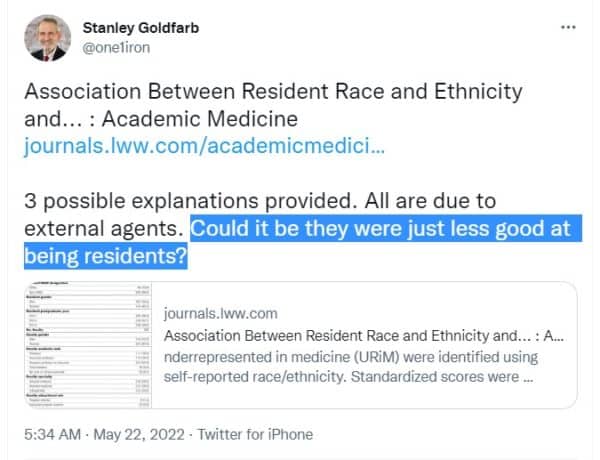
The entire medical profession is too terrified to denounce this rubbish – with one exception, it seems. Dr. Stanley Goldfarb of Penn Medical School read the article about bad ratings for black and Hispanic residents.
He tweeted: “Could it be they were just less good at being residents?”
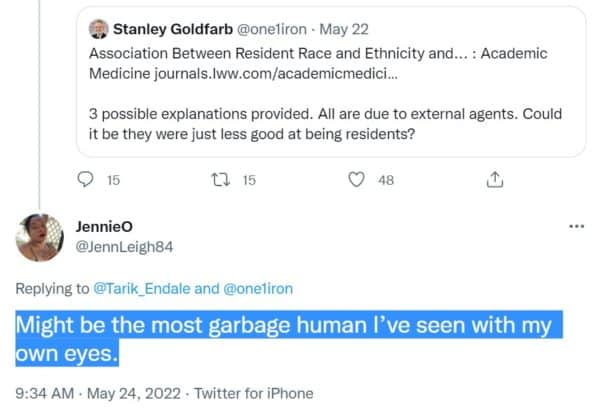
Horrors! Impossible! One twitter user said Dr. Goldfarb “might be the most garbage human I’ve seen with my own eyes.”
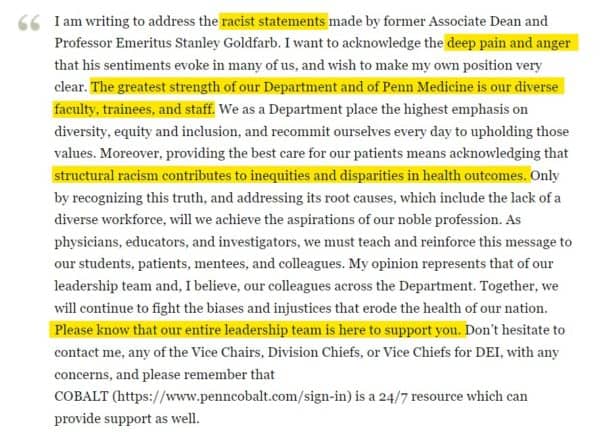
Within hours of his tweet, the dean of Dr. Goldfarb’s medical school emailed all students and faculty a classic of self-righteousness and bootlicking:
He deplored Dr. Goldfarb’s “racist statements,” and acknowledged the “deep pain and anger” they had caused. He claimed the medical school’s greatest strength was diversity and said structural racism makes non-whites sick. And he promised that the school’s “entire leadership team” was standing by to console the traumatized.
No. Those darling black and Hispanic residents could not have been lousy at their jobs! Needless to say, there is now a petition to remove Dr. Goldfarb from U Penn.
You see, he is guilty of other crimes.
He runs an organization called Do No Harm, which just-released a report called “Only DEI Advocates Need Apply.”
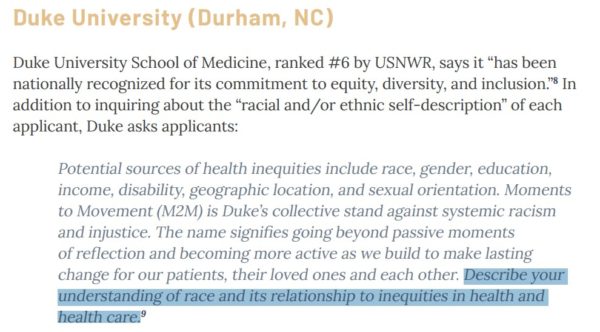
American medical schools make sure that applicants babble anti-racist claptrap. Duke University tells them: “Describe your understanding of race and its relationship to inequities in health and health care.”
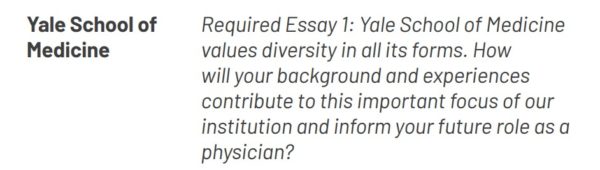
Yale has a “Required Essay: Yale School of Medicine values diversity in all its forms. How will your background and experiences contribute to this important focus of our institution and inform your future role as a physician?”
University of Minnesota: “Our country is reckoning with its history, racism, racial injustice, and especially anti-black racism. Please share your reflections on, experiences with, and greatest lessons learned about systemic racism.”
Anyone who says “There’s no such thing as systemic racism” has no chance of getting in. Only zombies need apply.
Med school is now as much about brainwashing as medicine. The Association of American Medical Colleges accredits medical schools and tells them what to teach. It has just published new standards in medical education: “Diversity, Equity, and Inclusion Competencies Across the Learning Continuum.”
Right on page two it insists on “improved integration of diversity, equity, inclusion, and anti-racism in medical education and training.”
This means “disrupt[ing] the perpetuation of racist ideologies and practices in all aspects of the curriculum, including teachers, learners, and content.”
Where’s the racism in neurology, anatomy, or pediatrics? Well, it turns out that every med school course is stuffed with white supremacy, colonization, institutional racism, interpersonal racism, structural racism, internalized racism, and countless other horrors. And, of course, doctors must learn that race is “a social construct that is a cause of health and health care inequities, not a risk factor for disease.”
Race is an excuse for white doctors to persecute blacks and Hispanics – but, somehow, not Asians. “Patients of color” are never sick because they are fat, miss appointments, forget to take medicine, can’t read, shoot each other, or because of genetic differences.
Med schools everywhere are turning their courses inside out. The medical program at University of Michigan has an “Anti-Racism Oversight Committee” which has issued an “Action Plan Report.”
It will “Identify practices that contribute to racism and discrimination” and will “Identify an approach that achieves an anti-racist culture and identify metrics to track the progress and outcomes.”
Metrics! How do you measure the success of an anti-racist culture? I shudder to think.
The American Medical Association has gone predictably nuts with an “Organizational Strategic Plan to Embed Racial Justice and Advance Health Equity.”
It’s not joking about “equity.” In 86 pages of twaddle, it uses the word 454 times. It also blasts “the myth of meritocracy. A narrative that attributes success or failure to individual abilities and merits.”
Last year, the National Institutes of Health – the biggest medical grant-maker in the US by far – announced that “NIH leaders detail commitment to end structural racism in biomedical science.”
A gigantic task! You can imagine the pork, baloney, and glassy-eyed piety in all this. But if you apply for a grant, you have to promise to spend the money fighting cis-hetero-white-normativity. Finding a cure for something will be an unexpected bonus.
Ultimately, fighting structural racism means deliberately treating preferred minorities better than whites. This first came to attention during Covid: “Food and Drug Administration Guidance Drives Racial Rationing of COVID Drugs.”
The FDA said that giving scarce drugs to blacks and Hispanics first compensates them for “systematic health and social inequities.”
Two Boston doctors have come up with “An Antiracist Agenda for Medicine,” in which they say that colorblind medical treatment isn’t good enough.
There must be “medical restitution, which must be pursued at the institutional level.”
This means “centering black and Latinx patients” — deliberately giving them better treatment.
And whitey better keep his mouth shut. Dr. Edward Livingston used to be one of the top editors at the once-prestigious Journal of the American Medical Association, but not anymore: “JAMA Editor Resigns Over Controversial Podcast.”
What did the poor boy say? “Structural racism is an unfortunate term. Personally, I think taking racism out of the conversation will help. Many of us are offended by the concept that we are racist.”
How dare a white man think he’s not racist? He was out quick as a wink, and JAMA officially pronounced his words “inaccurate, offensive, hurtful and inconsistent with the standards of JAMA.” JAMA’s standards? “Structural racism is real, pernicious and pervasive in health care.”
And so the top editor had to grovel and resign, too.
Guess who’s the new editor-in-chief? Kirsten Bibbins-Domingo, a black woman, a “DEI Champion” who specializes in “health inequity.”
She’ll whip those sorry white men into line.
This is what white people get for their unspeakable cowardice. They must never defend themselves. They must confess perpetual guilt. They must turn their institutions – and their jobs – over to people who built their careers on resentment. And white doctors will help build a system in which their own people will be at the back of the bus for treatment.
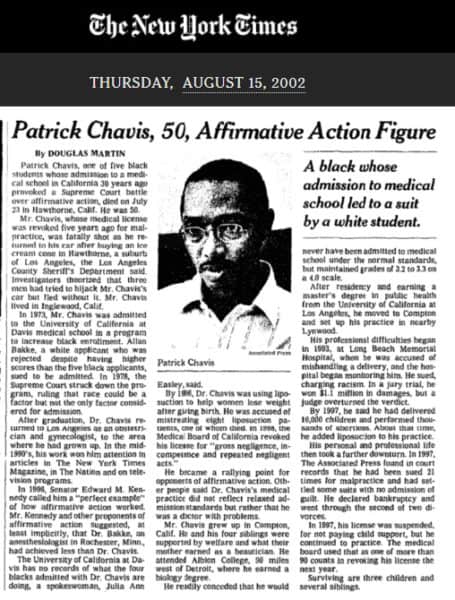
And some of it we saw so long ago. Patrick Chavis went to UC Davis Medical School in 1973 under a program to let in underqualified blacks.
He became a doctor but the New York Times was surprisingly frank about his sad career.
At first he was heralded as the great black hope. In 1996, Senator Ted Kennedy called him “the perfect example” of how affirmative action should work. In fact, he bungled so many operations he was sued 21 times for malpractice. The year after Kennedy praised him, California suspended his medical license, saying he had an “inability to perform some of the most basic duties required of a physician.” He kept doing surgery anyway, and one of his patients bled to death. Twenty years ago, someone shot and killed him. Robbery? Carjacking? Angry former patient? The crime was never solved.
Are white people utterly incapable of learning? I think I’ll send a contribution to Stanley Goldfarb’s organization.
















No comments:
Post a Comment